President’s essay
When SARS-CoV-2 (coronavirus) spread throughout the world, 2020 immediately became a historic year. The virus recognized no boundaries; neither physical nor political. Our Cold Spring Harbor Asia conference center employees in Suzhou, China, were the first affected by the pandemic, and soon thereafter, in March, we faced COVID-19 in New York. Like people everywhere, Cold Spring Harbor Laboratory (CSHL) confronted the same challenges: how to continue our work and our lives while keeping healthy and safe. Beyond this, the Laboratory’s scientists, educators, and administrators felt an extra responsibility to use our knowledge and resources to further scientific understanding of the new virus, but also to continue our important research and educational programs, since diseases like cancer and mental health conditions still need progress. The main challenge was how to balance these challenges while limiting SARS-CoV-2 exposure to our employees and their families.
Research activities at CSHL never stopped, though we did have to limit activities on the two research campuses as we formulated policies and protocols to ensure a safe working environment. We needed to comply with rapidly changing orders from state, county, and local authorities as New York became an early epicenter of the pandemic. Conflicting priorities among these local and federal agencies and a lack of clear national response further complicated matters as we strived to communicate with our employees about where to turn for reliable information about the pandemic.
Most of our administrative staff has been able to work from home, but dozens of essential workers, including mailroom, buildings and grounds maintenance, information technology (IT), partial culinary, and research core facilities staff continued to come to campus and keep our facilities running efficiently. The Human Resources and Communications departments kept our employees informed of new policies. Our scientists juggled schedules and experiments to keep their research going and their postdocs, students, and technicians safe. The ability to continue limited research was aided by the distributed nature of our small research buildings scattered throughout the large campus, thereby limiting the number of people in a particular building. Throughout the year, we received encouragement and much-needed funding from both long-time and new friends, even without the usual calendar of fund-raising events.
Programs pivoted
A full scientific conference calendar was already under way in early 2020 when the virus abruptly made large gatherings and travel risky activities. Executive Director David Stewart and his Meetings & Courses Program staff responded quickly and developed our first fully virtual programs, beginning with a Systems Biology meeting in March that brought together more than 170 participants for Zoom presentations and digital poster sessions. By the end of the year, CSHL had pioneered a new approach to virtual scientific exchange. We hosted five virtual courses and 26 virtual meetings in 2020, including a series specifically devoted to COVID-19. More than 14,000 scientists around the world joined us for these virtual events. These virtual meetings also enabled participation by scientists from countries not normally represented at our in-person meetings. As a consequence, a hybrid meeting involving both in-person and remote attendance will be the norm even after the pandemic is long gone.
Likewise, the DNA Learning Center (DNALC) was forced to suspend in-person school visits and on-site educational programs in March. Executive Director Dave Micklos and his team pivoted to alternatives that could support both at-home and classroom learning from a distance. The DNALC developed webinars, virtual field trips, and science clubs to keep students engaged. The first of these programs responded to the needs of teachers and students through our initiatives in China. By the end of 2020, our educators had converted their hands-on curriculum into 100 new videos, accompanied by kits students could use at home—or anywhere in the world. They manufactured and sent out 3,000 home science kits, continuing to serve the 30,000 students they usually serve in the New York metropolitan region every year. Their YouTube video curriculum was viewed 1.6 million times during the pandemic, almost doubling their previous viewership.
While we shifted our activities to keep these programs going, one service provided by CSHL already was uniquely positioned to serve when the pandemic hit: our preprint servers, bioRxiv and medRxiv. CSHL Press Director John Inglis and Assistant Director Richard Sever created bioRxiv in 2013 to accelerate science by providing a place for researchers to share basic research findings in the life sciences in advance of the often-protracted peer-review process of publishing in a research journal. In 2019, they launched medRxiv, which we operate in partnership with the BMJ journal and Yale University, to do the same for clinical research. It often takes a full year for submissions to work their way through the process of publishing in scientific journals, and with COVID-19 cases growing exponentially, no one had that time to wait.
The science itself was happening fast, but unless new findings about SARS-CoV-2 and the disease it caused were shared quickly, other researchers would be unable to build on that knowledge. Not surprisingly, use of our preprint servers surged during the pandemic. As of this writing, over 15,500 papers on COVID-19 and SARS-CoV-2 have been published on medRxiv and bioRxiv. This helped drive the science that improved management of COVID-19, shaped public health policies, and delivered multiple vaccines against the virus in record time. Now that the scientific community has come to rely on this rapid exchange of information, we expect bioRxiv and medRxiv use will remain high, even after SARS-CoV-2 eventually becomes less pervasive in our lives.
Science matters
Probably more than any event in our lifetimes, COVID-19 has highlighted to the public the importance of scientific research. While researchers in a variety of disciplines have worked tirelessly to advance our understanding of this particular viral syndrome, it’s important to note that our response to the spread of SARS-CoV-2 builds on a long history of basic science, including some done right here at CSHL.
In January, before SARS-CoV-2 had even been detected in the United States, the viral genome had been sequenced and shared. That achievement was essential for testing for the virus, tracking its spread, and recognizing emerging variants. It was enabled by many basic science advances made in the last 50 years, including many that were recognized with Nobel Prizes, from the discovery of messenger RNA, the discovery of RNA producing enzymes, and the development of methods to manipulate DNA and RNA and determine their sequences and the structures of the proteins they encode.
Studies of the basic biology of the immune system paved the way for recognizing the extreme inflammatory response some patients experience when they are infected with the virus, and for developing a monoclonal antibody cocktail as a treatment for COVID-19. The first two vaccines approved in the United States, developed and tested in less than a year, use lipid-packaged messenger RNA to direct our cells to produce one of SARS-CoV-2’s proteins, thereby training the immune system to recognize and respond to the virus. This innovative approach also builds on fundamental science, including the discovery of messenger RNA in 1961.
The single-dose vaccine developed by Johnson & Johnson in collaboration with Beth Israel Deaconess Medical Center also directs the body to produce an immune-stimulating viral protein. In this case, the instructions are encoded in DNA and delivered to cells using a modified adenovirus as a vector. CSHL scientists, myself included, studied adenoviruses extensively in the 1970s and 80s, primarily for cancer research. Terri Grodzicker, who is now our dean of academic affairs, Yasha Gluzman, and Robert Tjian developed adenovirus vectors to deliver genetic instructions to human cells to direct them to produce a foreign protein. In my lab, we figured out how to grow the human cells used for this system in suspension culture rather than on plastic dishes, so adenovirus could be produced on a much larger scale. The cells and viruses have been modified over the years, but adenovirus vectors got their start here at CSHL and are now part of approved vaccines for COVID-19.
COVID-19 research
As these examples illustrate, we can’t fully appreciate in the present how the fundamental discoveries our scientists are making might be used in the future. But I’d like to highlight some ways in which CSHL researchers have contributed directly to addressing the current crisis. Regardless of what their labs were studying when the pandemic hit, many of our researchers readily pivoted to investigating the virus and its effects.
One area of intense focus for those working to rein in the effects of SARS-CoV-2 has been the virus’s spike protein, which it uses to infiltrate host cells. This is the protein now targeted by vaccines and experimental therapies. Early in the pandemic, the availability of these proteins was limited, so several CSHL laboratories, including Leemor Joshua-Tor’s, devoted resources and time to producing large amounts for the research community.
Along with chemist John Moses, Joshua-Tor has also been working on developing potential antiviral compounds to combat SARS-CoV-2. Moses, one of our newest faculty members, is synthesizing chemicals that may be able to halt infection by blocking one of the virus’s essential enzymes. Nicholas Tonks, a cancer biologist, is exploring the possibility of repurposing an existing cancer drug to control the extreme inflammation that the virus can sometimes cause.
CSHL scientists have been investigating whether famotidine, an existing drug used to treat heartburn, can reduce the severity of COVID-19. Tobias Janowitz, an oncologist and cancer biologist, and David Tuveson, director of the CSHL Cancer Center, developed an approach that allows patients to participate in a clinical trial evaluating the drug from home, keeping people with mild or moderate cases of COVID-19 away from already strained healthcare settings. Participants monitor their own vital signs and report their symptoms daily via an Apple iPad, and changes are tracked to evaluate the efficacy of the drug. An entirely virtual Phase II trial, completed in collaboration with Northwell Health’s Feinstein Institutes for Medical Research, began recruiting participants in January 2021. While this self-reporting paradigm is particularly valuable during the pandemic, it could also become useful for future clinical trials treating cancer and other conditions.
As New York’s largest health system, Northwell has now treated more than 100,000 patients with COVID-19. CSHL established an affiliation with Northwell in 2015, aiming to accelerate the translation of our discoveries in cancer biology into better treatments and diagnoses for patients. This spring, CSHL scientist Partha Mitra leveraged this relationship to track COVID-19’s spread through the state with zip-code–level granularity. By analyzing data from more than 46,000 people whom Northwell tested for the virus in March and April, Mitra and his collaborators were able to show that the infection was already widespread in the metropolitan area when testing became available. Their analysis further identified regions and demographic groups where infection rates were highest.
While working from home early during the pandemic, CSHL Fellow Jason Sheltzer and collaborator Joan Smith, an engineer at Google, made important discoveries about the ACE2 receptor on the surface of human cells that SARS-CoV-2 uses to get inside. Using data from previous studies, they found evidence that cigarette smoke drives cells to make more of this receptor—thus creating more access points for the virus. This may explain why people who smoke are among those who are most vulnerable to infection with SARS-CoV-2.
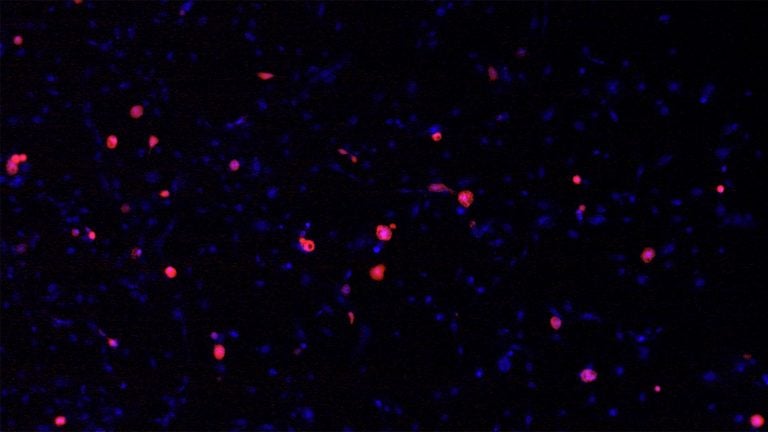
Finally, cancer biologist Mikala Egeblad has organized a global network of clinicians and scientists to investigate a possible cause of the lung damage that occurs in extreme cases of COVID-19: sticky, web-like structures generated by the immune system called neutrophil extracellular traps, or NETs. NETs help fight infection by capturing bacteria, but excess NETs, which Egeblad had been studying because of their role in cancer metastasis, can damage organs and may contribute to acute respiratory distress syndrome and thrombosis. Egeblad and her collaborators have found NETs in the lungs of patients who died of COVID-19 and think they may be responsible for dangerous blood clots. Several clinical trials are now investigating whether it’s possible to block NETs with drugs to improve outcomes for patients with COVID-19.
Preparing for the future
While we work to address the current crisis, we’re also aware that we need to prepare for the future. We almost certainly will experience new medical emergencies, including but not limited to the emergence of other dangerous pathogens. One thing that particularly concerns me is the growing problem of bacterial antibiotic resistance. CSHL has been hosting meetings on microbial pathogenesis since the 1940s. And the nation will need to re-think approaches to these pathogens and amplify support for research aimed at dealing with infectious bacteria that no longer respond to our existing arsenal of drugs.
Regardless of what crisis we face next, it’s clear from the devastating way the COVID-19 pandemic has progressed and persisted that we’ll need strong national leadership and coordination. A nationwide, Federal coordinating body should be in place for all future medical emergencies to oversee national, state, and local health agencies, to set policies, and to secure and distribute essential supplies, even engaging the armed services in a more effective way. And these actions must be supported by sound science. CSHL’s research and educational programs are helping to ensure that science will be ready. Rebecca Leshan, the executive director of the CSHL Banbury Center, is planning strategy sessions for policy-makers on how to address future health threats. I am committed to connecting science with society and preparing better for the potential health and medical risks of the future.
Bruce Stillman, Ph.D.
President & CEO