Cold Spring Harbor, NY — The work of a team of scientists at Cold Spring Harbor Laboratory (CSHL) led by Professor Nicholas Tonks FRS, suggests a way to overcome one of the major technical obstacles preventing a leading therapeutic target for diabetes and obesity from being addressed successfully by novel drugs.
The target is an enzyme called PTP1B, discovered by Tonks in 1988 and long known to be an important player in the signaling pathway within cells that regulates the response to insulin. Insulin is a hormone that regulates carbohydrate and fat metabolism by spurring cells, particularly in the liver and muscle, to absorb glucose from the bloodstream and store it away for later use.
Insulin exerts its effects by binding to a receptor on the surface of a cell. This receptor then triggers a signaling cascade that involves sequential chemical reactions in which phosphate is added to target proteins by enzymes called kinases. In fact, the insulin receptor is itself a kinase that phosphorylates target proteins on specific tyrosine residues. Phosphorylation of this amino acid in target proteins serves as a switch to regulate function, thereby transmitting the effects of insulin to the machinery of the cell. The effects of the insulin receptor are countered by members of a family of enzymes called the protein tyrosine phosphatases (PTPs), which take the phosphate group back off tyrosine residues in proteins. Of particular importance to the regulation of insulin signaling is the phosphatase PTP1B.
“Type 2 Diabetes, the most common form, is a disease of insulin resistance,” Tonks explains. “In the disease state, an insulin molecule docks at a cell, but the cellular mechanism that sends its signal does not work properly. This is why simply adding more insulin will not solve the problem. What you really need to do is to promote insulin signaling within the cell—to favor the phosphorylation events triggered by the insulin receptor.”
For over a decade, scientists have known that when PTP1B is suppressed in mice by “knocking out” the gene that encodes it, the mice are rendered seemingly resistant to obesity induced by a diet that is high in carbohydrate and fat; importantly, these mice show increased sensitivity to the beneficial effects of insulin and do not develop diabetes. This suggests that generating a drug-like inhibitor of PTP1B may be an effective approach to restoring a normal response in insulin-resistant, diabetic patients.
The question for drug developers has been how to suppress PTP1B in people, in the specific context of its role in the insulin signaling pathway. Gene knockouts in humans, whether in specific cell types or systemically, are not possible with current technology. Furthermore, a variety of obstacles have also prevented scientists from inhibiting PTP1B biochemically with small-molecule drugs.
Previous studies by the laboratories of Professor Tonks and his colleague Professor David Barford have defined the three-dimensional structure of PTP1B. From this, they know that the active site of the enzyme—the place on the molecule where the removal of phosphate from target substrates is catalyzed—is a deep cleft.
“The development of molecules that block the active site, and thereby inhibit the function of an enzyme, is a standard strategy for drug design,” Tonks explains. “However, this deep active-site cleft in PTP1B has presented a major challenge to drug developers because it is highly charged. Consequently, any small molecules that bind there efficiently tend also to be highly charged and so will not get across cell membranes. This limits their drug development potential.”
Now Tonks and his team have identified a new targeting approach that sidesteps some of the key impediments encountered in trying to develop an active site-directed, drug-like PTP1B inhibitor. The approach is described in a paper published today in the journal Cell.
Tonks explains: “By analogy with driving a car, when insulin binds to its receptor on the cell surface the activation of the kinase initiates phosphorylation events that serve to hit the accelerator and start the response moving forward; however, the presence of active phosphatases means that the cell also has its foot on the brake, and enzymes like PTP1B try to slow the process down. Nature has devised an elegant mechanism to coordinate and fine-tune these competing effects.
“One of the responses of a cell to insulin involves the production of small amounts of a molecule we normally think of as highly corrosive: hydrogen peroxide (H2O2). Under the tightly regulated conditions of insulin signaling, H2O2 actually provides beneficial effects.”
Tonks’ team has demonstrated that the role of H2O2 in the cascade is to travel down into the active site cleft and oxidize a particular amino acid, a specific cysteine residue that is essential for the activity of PTP1B, thereby switching off phosphatase activity. Therefore, oxidation of PTP1B following insulin stimulation temporarily holds the phosphatase in an inactive state, removing its ability to switch off the signaling pathway and so allowing the cell to “take its foot off the brake.”
Ultimately, PTP1B is reduced and reactivated so that the signaling response to insulin can be terminated, returning the system to its ground state. This raises the question of whether it is possible to stabilize this oxidized form of PTP1B so that the phosphatase is maintained in an inactive condition, allowing a more robust and prolonged signaling response to insulin that would address the resistance to the hormone that is found in diabetics.
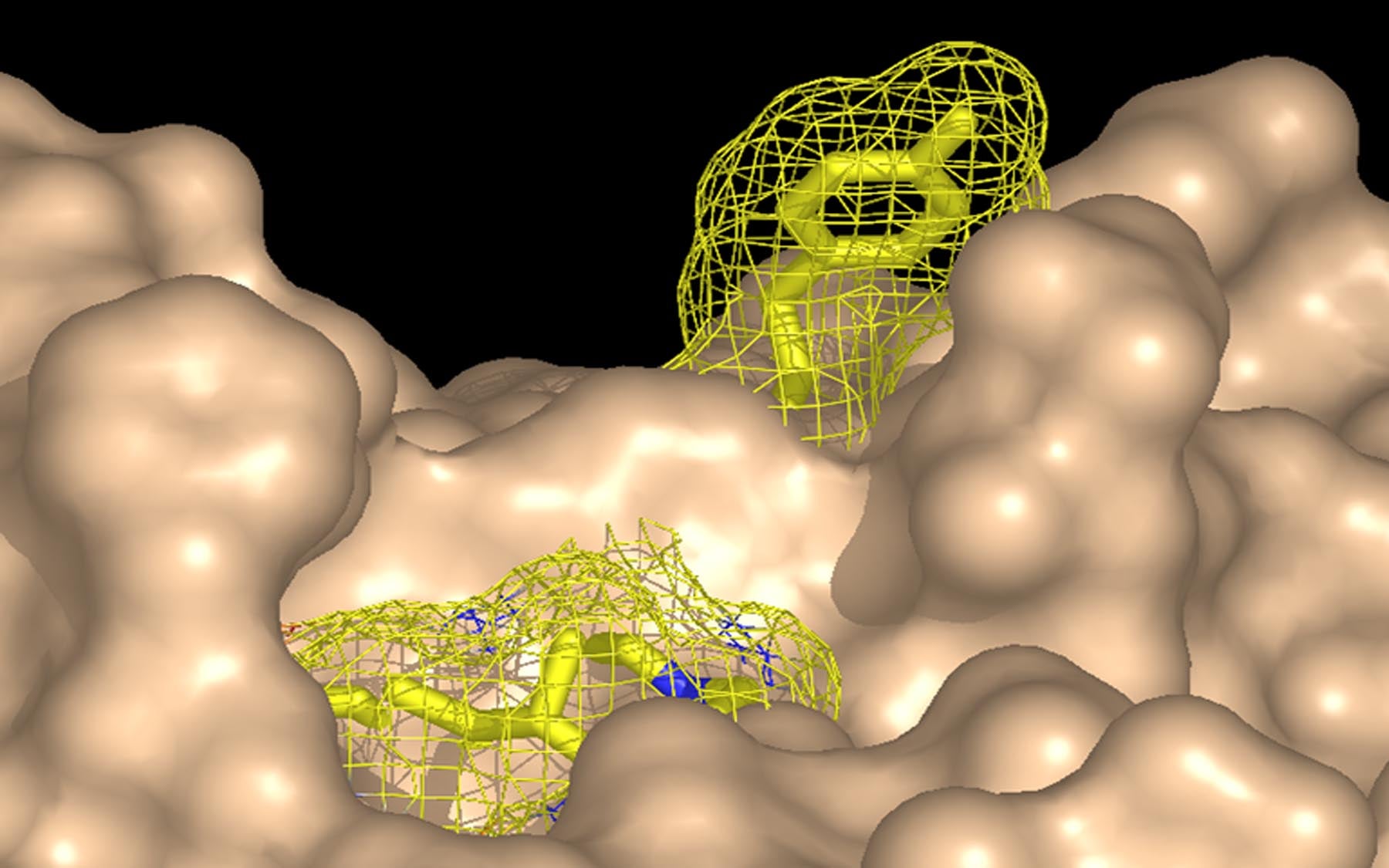
A key insight of Tonks’ team was that oxidation induced profound changes in the conformation, or shape, of the PTP1B molecule in which the active-site cleft splays open and its constituent parts are then presented on the surface of the protein. This profound conformational change in PTP1B generates an inactive form of the enzyme in which the problematic, charged properties of the active site have been removed and unique potential binding sites for drugs are presented, which are not found in the native, active enzyme.
In experiments reported in the Cell paper and performed by Aftabul Haque, a graduate student in the Tonks lab from the MCB Program at Stony Brook University, the team designed a strategy through which they generated recombinant antibody constructs that recognized specifically this oxidized, inactive form of PTP1B. Following expression in cells, these recombinant antibodies specifically sequestered and stabilized the oxidized form of PTP1B that is produced in response to insulin. Most importantly, expression of these antibodies resulted in the hoped-for enhanced and prolonged signaling response to insulin.
One major technical problem remains. Although these antibodies display the ability to promote insulin signaling, it is extremely difficult to deliver antibodies to the interior of cells as drugs using current biotechnology. Although there are effective antibody therapeutics for other diseases, they tend to be delivered via injection and attach to receptors on the outside of target cells. Therefore, if these new insights about targeting PTP1B are to be of practical use in the near term, Tonks says, a small molecule must be found that has the same effect on PTP1B as the antibodies identified in the team’s experiments.
The search for such a molecule has now begun.
Written by: Peter Tarr, Senior Science Writer | publicaffairs@cshl.edu | 516-367-8455
Citation
“Conformation-Sensing Antibodies Stabilize the Oxidized Form of PTP1B and Inhibit its Phosphatase Activity” is published September 29, 2011 in Cell. The authors are: Aftabul Haque, Jannik N. Andersen, Annette Salmeen, David Barford and Nicholas K. Tonks. The paper can be accessed online at: doi:10.1016/j.cell.2011.08.036
Principal Investigator

Nicholas Tonks
Professor
Caryl Boies Professor of Cancer Research
Cancer Center Associate Director of Shared Resources
Ph.D., University of Dundee, 1985