Base Pairs podcast
Many stories start the same. Boy meets girl, they fall in love, and there’s a happy ending. In the story of Elizabeth “Bessie” Dashiell, that boy was John D. Rockefeller, Jr., and by all accounts they should have gotten their happily-ever-after. But Bessie was in a minor accident, getting her hand caught in between the seats of a train car.
This injury was just the tip of the iceberg for Bessie. The pain persisted for months, so she wound up in the office of up-and-coming surgeon William B. Coley to find the remedy. Unfortunately, Dr. Coley discovered something far worse than a damaged muscle or broken bones: a tumor that had been growing since before the accident. In spite of all his efforts to save his patient, including surgically removing Bessie’s hand, Dr. Coley wasn’t able to stop the metastasis of Bessie’s aggressive cancer. The young sweetheart of the heir to the Rockefeller fortune passed away in 1891, at the age of 18.

But Bessie’s end was the beginning of another story, one about a new kind of treatment for cancer called immunotherapy. It involves mobilizing one’s own immune system to fight tumors, and encompasses several different types of treatments. Its history is a long and storied one, with scientists today driving the field forward at a pace that has captured the public’s imagination–especially for those who have or are close to those who have cancer.
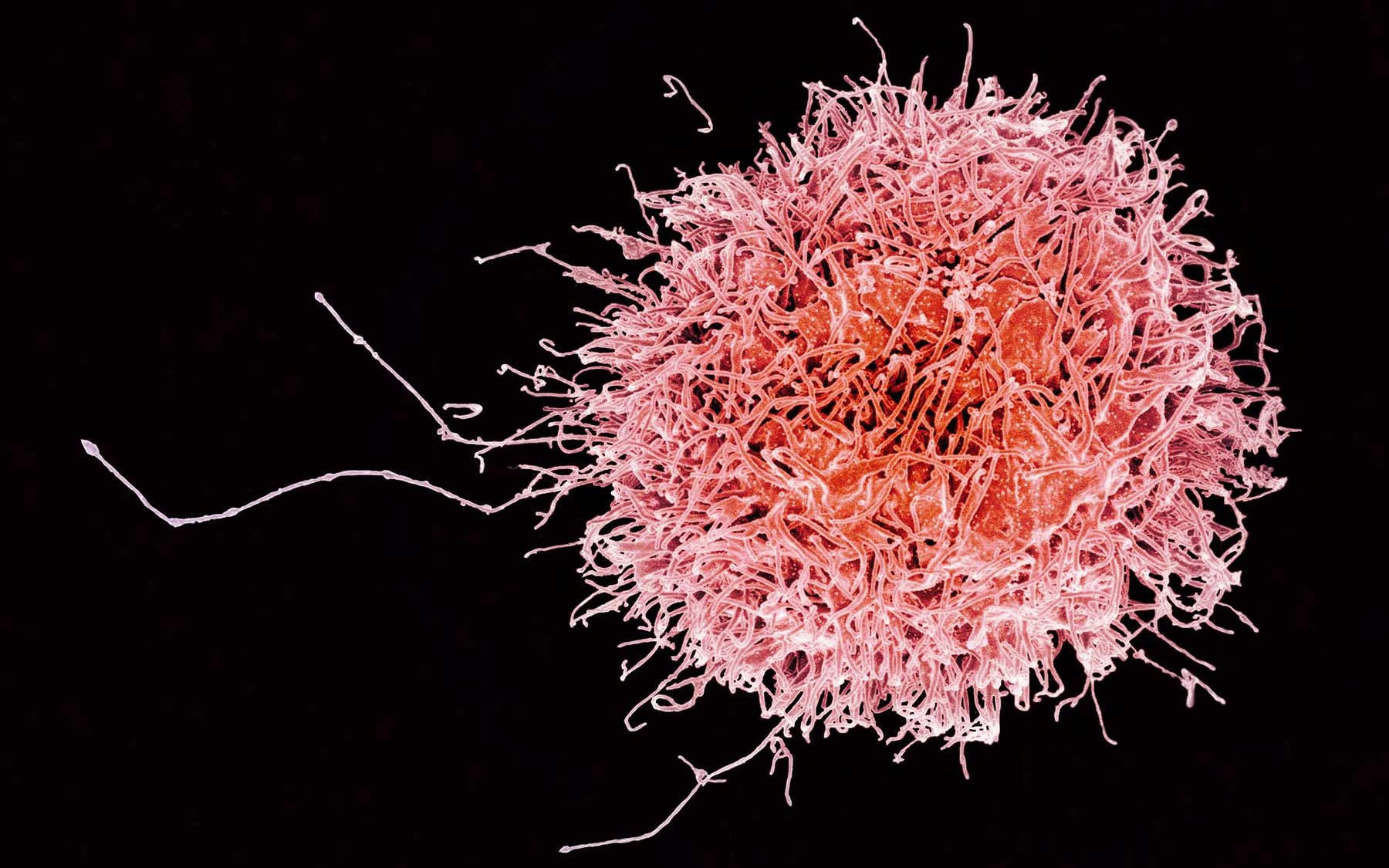
Remarkable methods have been tested, and in several cases marketed, that stimulate the patient’s immune system to fight back against cancer. CSHL Professor Doug Fearon has been exploring how cancer hides in plain sight from our immune cells. Especially killer T cells. He and colleagues are testing a drug combination designed to reveal cancer cells to the immune system, allowing T cells to destroy the cancer cells in their midst.
So how did a simple hand injury lead to the uncovering a fundamental principle of immunotherapy, which researchers like Doug Fearon are finally beginning to master? Listen to the eye-opening tale, and get some deeper insights into the state of immunotherapy research today. It’s all in the latest episode of Base Pairs.
AA: And I’m Andrea,
BS: And this is Base Pairs.
AA: The power of genetic information has helped reveal many new treatment approaches to cancer, including a whole class of treatments known as cancer immunotherapies… or, so I thought at least. I was under the impression that cancer immunotherapy—which uses the body’s own immune system to fight cancer—was fairly new. But Brian told me that’s not the case.
BS: Yeah, I know you’ve been talking to a scientist who used genetic information to find a new cancer immunotherapy, which we’ll get to later. But first, I have a story from way before anyone even knew that DNA is the genetic material. It starts back in 1890 with a young woman named Elizabeth Dashiell. Her friends called her Bessie.
BS: Bessie is a young lady, about 17 at the time, and she’s been traveling for summer vacation. She’s excited because she’s befriended a well-off young man who, by all accounts, has taken quite a liking to her. His name is John D Rockefeller Junior,
AA: So if you know a thing or two about U.S. history, you know that things are looking up for Miss Dashiell.
BS: However… as with many memorable stories… this is when disaster rears its ugly head.
PC: “She had injured her hand in a Pullman car jolting.”
BS: That, I should say, is Pete Coley, and we’ll get to where he fits into all this in a second.
AA: Ok, so something bad happened to Bessie, but before you continue… what’s a Pullman car?
BS: Aha yea. Basically, Bessie got her hand stuck between seats in a train car when it violently shook.
AA: Ahhh.
BS: So, months later, the pain from that train car accident is still there. Bessie knows something is wrong and finds herself a surgeon in New York City – a man by the name of William B. Coley.
AA: Oh ok. And how is Pete related?
BS: William was Pete’s grandfather and an up-and-coming surgeon. However, when he examined his young patient, he found something unexpected on that injured hand. What had actually been causing Bessie’s persistent pain was something unrelated to the accident. It was something much-much worse.
AA: What… what was wrong?
BS: Well, Coley knew a bone tumor, called a sarcoma, when he saw one.
PC: “He removed her hand, and tried to save her with surgery, which is was the only thing going in those days.”
BS: But it wasn’t enough. The aggressive cancer spread from Bessie’s limb to the rest of her body, harrying the young girl with painful tumors. All Coley could do was make his patient comfortable, and in 1891, Bessie Dashiell died at the age of 18.
AA: Sheesh. Well, I’ve heard stories like this before, and I can guess where it leads. Coley was frustrated with how powerless he was and… I’m guessing he sets out to improve cancer treatment options?
BS: You nailed it! But uh… this is where the story gets… dark.
AA: I’m pretty sure this was already SUPER SAD, Brian.
BS: Ok but darker. Like… mad scientist dark. Fast forward ten years later, and you’ve got an obsessive William B. Coley walking into hospitals, looking for the sickest, most near-death cancer patients. He’d slice them with a scalpel and then rub a hodgepodge cocktail of bacteria into the wounds.
AA: What?! Why?! You’re right! That does sound mad! Why did no one stop him?!
PC: “He got in trouble almost all of his life but — he had a great reputation for integrity. — Fortunately — he did end up friends to the Rockefellers and a few of his patients. — He, had to be a really live wire guy as well as likable or else none of this would have happened.”
BS: And Coley wasn’t only likable. People trusted in what he was doing, because believe it or not, he was onto something. Coley was chasing after what doctors at the time simply called “spontaneous regression” – rare but documented moments when the tumors of a cancer patient simply disappeared overnight.
PC: “He began to research the case histories in New York, especially, and he got people all around the world to try to find out what was the trigger for this. And, they found that if there was an infection of some kind – it could be, almost any infection… And with a big temperature, and a big response — miraculously — cancer disappeared.”
BS: He first discovered an example of this phenomenon in the case of a German immigrant simply called “Stein.” Years before Colley’s failure to save Bessie, Mr. Stein had been admitted to New York Hospital with a sarcoma very similar to hers. However, unlike the tragedy of Bessie Dashiell, Stein walked out of the hospital disease free only a few days later.
AA: That definitely sounds like spontaneous regression. So, I’m guessing Stein was hit with some kind of fever, like Pete described.
BS: Through some medical record sleuthing, Coley learned that Stein had come down with a severe post-operative skin infection. Remember, this occurred during the late 19th century – when the idea of germs was JUST becoming popular – so many surgeons weren’t even carefully washing their hands just yet.
AA: But fortunately, for Stein, this worked out to his benefit. By getting infected, he somehow was able to beat his cancer.
BS: Crazy, right? Coley even tracked the man down to a neighborhood in New York’s lower east side. Years after developing sarcoma, there Stein was, with no sign of the cancer save for a scar on his neck.
AA: So, Coley surmised that the bacterial infection had somehow caused the tumor to regress… and decided to start purposely inducing infections?
BS: The first cocktail he whipped up mostly contained the streptococcal bacteria –
AA: that’s the bacteria that causes strep throat
BS: – but Coley experimented with other infectious agents as well. He called the mixture “Coley’s Toxins,” and according to his records, it was remarkably effective when it worked.
PC: “It’s like being run over by a locomotive. I mean, wam-o! And you’d have this huge temperature. And the sweats and feel like you’re dying of you know, typhoid fever or something like that. Which was a sign, that you know, that the immune system had activated. I mean it’s a little… it was a pretty crude way of knocking the door down, but it opened up the immune system.”
AA: Ah! So, the infection from Coley’s Toxins was basically jump-starting the immune system – sort of waking it up to go fight off the bacteria and in the process, it also could attack the cancer. That’s super clever! And yet, it doesn’t sound like Coley knew that this was what was happening….
PC: “Yeah. — He had no idea what he was doing. He had NO idea what he was doing — Nobody at the time understood that there was an immune system. All the doctors in the world had never dreamed of it.”
BS: It’s important to point out that a fascination with what would eventually evolve into a study of cancer and the immune system persisted in Coley’s family. In the mid 1900s, his daughter Helen discovered 3,000 of Coley’s case studies in the family barn and soon after became one of the first champions of immunotherapy, founding the Cancer Research Institute. And Pete’s father, Bradley Sr, continued to use a refined version of the Toxins at Memorial Hospital well into the 1950s. Remarkably, some of his patients are still alive today thanks to this treatment!
AA: Immunotherapy got its start through trial and error, because so little was known about the immune system at the time. But in the century since Coley applied the first cancer immunotherapy, scientists have learned a whole lot more about how the immune system works.
DF: If the problem in cancer immunology is turning on the immune system, well, we know the rules for that.
AA: That’s Professor Douglas Fearon, who runs a cancer research lab here at CSHL and has dedicated much of his 50-year career to learning what he likes to call the “rules of the immune system.”
BS: Lack of understanding of those rules is why most of our listeners probably have never heard of Coley’s Toxins until now. The toxins worked in some patients but not others, and since no one knew why, it quickly became overshadowed by another up-and-coming cancer treatment: chemotherapy.
AA: Happily, Doug is closing in on a new cancer immunotherapy—one that doesn’t use unpredictable infections, nor is it like the poisonous chemotherapies that are still used to treat cancer today. It’s being tested in both colorectal cancer and pancreatic cancer patients right now. Doug and his team came up with the idea for this cancer immunotherapy by using genetic information and other tools to figure out how to use the rules of the immune system to their advantage.
DF: If you understand the rules that govern the immune system, then you can imagine these manipulations for immunotherapy.
BS: That’s really different from how Coley developed his immunotherapy. He had a hunch, and while a lot of work went into validating that hunch, its success also involved quite a bit of luck.
AA: Coley had a sense that if you can activate the body’s natural defense, it might be able to fight cancer. But after decades of studying what we now know as the immune system, Doug believes that it is already trying to attack the cancer, in many cases.
DF: I’m predicting that we will find that most patients have an ongoing immune response against their tumors.
BS: Really? Then what’s stopping their immune systems from just killing the cancer?
AA: Something that I found pretty mind-blowing. Cancer is evil, but sometimes I can’t help being impressed by its resourceful tactics. Research from Doug and other scientists suggests that the cancer disguises itself from the immune system—by tricking it into treating the tumor like a wound that needs to heal. attracting what biologists call growth factors, among other things, which in cancer is exactly what you DON’T want to happen!
DF: Maybe the problem is that the body thinks the tumor is a healing wound and it has to have mechanisms to protect the growing cancer cells. The body actually thinks that growing cancer cells is a regenerating tissue.
BS: Ok, I know that cancer is so difficult to defeat partly because it’s an invasion that comes from within. Genetic mutations in our own cells send them down the path to becoming cancerous, but they are still similar to healthy cells in many ways. So, the problem is that the immune system can’t detect the cancer cells because they look too similar to the healthy cells they started out as?
AA: That’s what I thought at first, too. But the disguise is more clever than that. I was amazed when Doug told me about just how sensitive the immune system is. For example, in humans, genes are usually thousands of letters long. If just one of those letters is wrong, like if a C becomes a G, that tiny change in the protein created from that gene is enough to set off an immune response.
DF: One point mutation, right. The immune system can see that as foreign.
BS: Wow, that really shows how good the immune system is at its job. And yet the cancer still outmaneuvers it.
AA: That’s part of why Doug is so confident that many cancer patients do have an immune response to their tumors, and that he just needs to remove whatever is getting in the immune system’s way.
BS: Ahhhh! And this is where learning the rules of the immune system must really help.
AA: Right. When Doug was based at Cambridge, he got interested in these cells called fibroblasts, which make structural materials like collagen—that stuff you often hear about in ads for beauty products. Fibroblasts are also critical in wound healing, and, curiously, are found in tumors.
BS: Many people don’t realize this, but tumors aren’t made up of only cancer cells. They contain lots of healthy cells too.
AA: Doug had his own hunch, though his was guided by much more knowledge of the immune system than Coley could have had. What if fibroblasts, these cells that help in healing wounds, were protecting the cancer cells?
DF: We made a mouse in which we could conditionally kill, at any point in time, the fibroblasts in the tumor. And we found if we did that, the immune system killed the tumor. So, the fibroblasts were immune-suppressive, that was the most unexpected finding. So, then we simply isolated the fibroblasts and said, “What genes are they expressing? How are they doing this?”
BS: Gene expression is kind of like a cellular activity log. It gives a sense of which genes the cell is using at any given moment.
AA: Yeah, and those tests revealed that the fibroblasts inside the tumor were making a particular molecule known to be involved in regenerating tissue, like what happens in wound-healing.
BS: That’s pretty suspicious.
AA: This is the really strange part. It seems that the cancer cells fashion their disguises out of this special molecular material that they get from fibroblast cells.
DF: Another cell in the tumor is making it, but the cancer cells are coating themselves, and this is somehow allowing them to prevent T-cells from coming into the cancer cell regions and attacking the cancer cells.
BS: That is both amazing and distressing.
AA: Fortunately, that new cancer immunotherapy drug we mentioned earlier prevents cancer cells from being able to put on this disguise. Now, Doug’s lab at CSHL is working on figuring out why this molecular cloaking device exists in the first place.
DF: This means by which tumors protect themselves from immune attack did not evolve for the sake of protecting tumors. — Part of my lab is trying to investigate what normal circumstance contributed to the evolution of this tissue protective pathway. That’s going to be relevant in thinking about the biology of the system, but also be very clinically relevant. We’ll need to deal with that in patients.
BS: Doug was a medical doctor before he was a research scientist, and he never loses sight of the fact that he’s doing research to benefit patients. Just like what happened with Coley, when Doug was practicing medicine, he felt like he was hitting a wall because he needed to know more about how the immune system works. Progress in medicine depends on improving our understanding of how the body works—and that comes from basic science.
AA: Yeah, Doug transitioned from being a doctor who treated patients to being a researcher in pursuit of discoveries that would lead to more effective treatments. For much of his career, Doug was actually more interested in turning off the immune system in autoimmune disease patients, instead of turning it on against cancer.
BS: How did he end up studying cancer, then?
AA: Well, treating autoimmune disease more effectively turned out to be an even harder problem than he had thought it would be.
DF: Around 2005, 2006, maybe a little bit earlier, I realized I was getting a bit old and I had not accomplished the deal I had made with myself: I will stop seeing patients so I can make a discovery that can affect the health of patients.
AA: As he was thinking about where his chances of affecting the health of patients were the greatest, something serendipitous happened. He was asked to serve on the Scientific Advisory Board for the Ludwig Institute for Cancer Research, so he read up on cancer to prepare.
DF: I started reading cancer immunology, and it was an eye opener! There were experiments done in the 1970s that allowed one to form hypotheses about why tumors escaped immune control, and I didn’t feel as though it was being followed up by current cancer immunologists. And I had an idea. — Maybe the fibroblasts are creating the immune suppressive microenvironment and instructing all of the immune cells to turn off. — And then, best of all, the idea was right!
BS: Doug is not a boastful guy at all—that is pure excitement about making a discovery that could help patients. But how did he turn that discovery into a treatment? If the fibroblasts are suppressing the immune system… does that mean these immune-boosting supplements we hear about all the time could help fight cancer?
AA: This immune-boosting craze came up when Doug gave a public lecture on immunotherapy here at CSHL with another doctor/researcher named Robert Maki. He’s one of the leaders of a strategic affiliation between CSHL and Northwell Health, New York State’s largest health care provider. Dr. Maki still sees patients regularly, and here’s what he had to say.
RM: The big question I’m always asked—I get this at least twice a clinic, a couple of times today, in fact—is how can I boost my immune system? And pretty clearly, the answer is you just call a cardiac surgeon. You know, Dr. Oz will be happy to tell you all of the good things that you can do to boost your immunity. [audience laughs]
BS: That was a good burn.
AA: It really was. For those who would like to find out which supplements actually have scientific evidence to back them up, Dr. Maki did also recommend something.
RM: Memorial Sloan Kettering have put together a very nice website called About Herbs, and this can tell you a lot about all of these natural products that people are taking.
AA: Anyway, instead of learning immune-boosting strategies from cardiac surgeons like Dr. Oz, Doug was learning from scientists who study viruses.
BS: Wait, what do viruses have to do with any of this?
AA: The cancer immunotherapy drug that Doug’s team developed and is now testing in clinical trials was actually first developed to fight HIV, the virus that causes AIDS. Dr. Maki explained that this really makes so much sense, because both viruses and cancer cells find ways to hide from the immune system.
RM: This is what viruses have been trying to do throughout evolution. So EBV, Epstein-Barr virus, which causes mononucleosis, has engineered itself, has been selected against being seen by the immune system. It’s really very much a stealth virus that has many ways of preventing the immune system from seeing it for example.
BS: HIV must be pretty stealthy too, since it’s so deadly when left untreated.
AA: Yeah, cancer is far from the only swindler out there trying to cheat the immune system. HIV uses a similar tactic to the cancer cells that Doug studies, and so do other viruses. He actually learned about the drug he’s now testing as a cancer immunotherapy when he was reading about West Nile virus.
DF: I said, “Geez, that’s kind of like what we want to do.” So, it was reading that paper that allowed me to choose that candidate — as regulating T-cell infiltration of the tumor.
BS: I would have never guessed that West Nile virus research could spark an idea for treating cancer. But that’s why basic research is so fascinating, and important—it’s how scientists come to make discoveries that they couldn’t have imagined in another context.
AA: Doug is all about that. He came to CSHL in part because the culture around here allows scientists to spend lots of time learning about all kinds of research in biology which helps them make valuable connections.
DF: You can’t design a life so you’re terribly efficient, you gotta have time to be inefficient, to read about things you don’t necessarily know you need to know, but that’s how you discover what you need to know.
BS: Finding out what you don’t know you need to know is quite a task. I’m glad Doug’s hard work looks like it’s paying off.
AA: The clinical trials are still in an early stage, but so far, so good.
DF: The clinical trial is the analysis of the tumors by looking to see how the drug changes the immune reaction of the tumor and the analysis is done by looking at gene changes and gene expression in tumor biopsies before and at the end of treatment, one week of treatment. — Our recent colorectal cancer patient trial suggests that — at least half the patients have T-cells that are coming in and killing cancer cells after our immunotherapy.
BS: That’s fantastic! T-cells are immune cells that are also sometimes called “killer” T-cells, because their job is to attack invaders. If they’re responding, that suggests the drug is getting the immune system to do its thing.
AA: It’s pretty exciting. Doug just recently got the trial with pancreatic cancer patients up and running, and hopes that this very hard-to-treat cancer will respond to the drug as well. But even if that shows success, scientists in his lab are going to keep studying this system, because…
DF: One actually can believe that if we understand how something is happening, we can maybe make it happen even better. So that’s what the work here, funded by the Lustgarten Foundation, is totally focused on.
BS: A scientist’s work is never done!
AA: That we know for sure.
Written by: Sara Roncero-Menendez, Media Strategist | publicaffairs@cshl.edu | 516-367-8455