Following up on Base Pairs 15, we learn how William Coley’s daughter used case notes to start the Cancer Research Institute. Professor Doug Fearon talks about on why the immune system identifies certain types of cancer cells more easily than others and we explore the might of the white blood cell in pop culture.
Transcript
BS: This is Base Pairs, the podcast about the power of genetic information.
Intro: Great scientific challenges, transcend national frontiers and national prejudices. For the language of science has always been universal.
BS: Hey, everybody. It’s Brian here.
AA: And Andrea.
BS: This is one of our Base Pairs chat episodes. We do these as a follow up to one of our more full storytelling episodes and in this case we’re following up an episode that we did about immunotherapy.
AA: Immunotherapy has kind of become a buzzword in the recent years in stories about say, former president Jimmy Carter who underwent immunotherapy and that seemed to have really helped him beat his cancer.
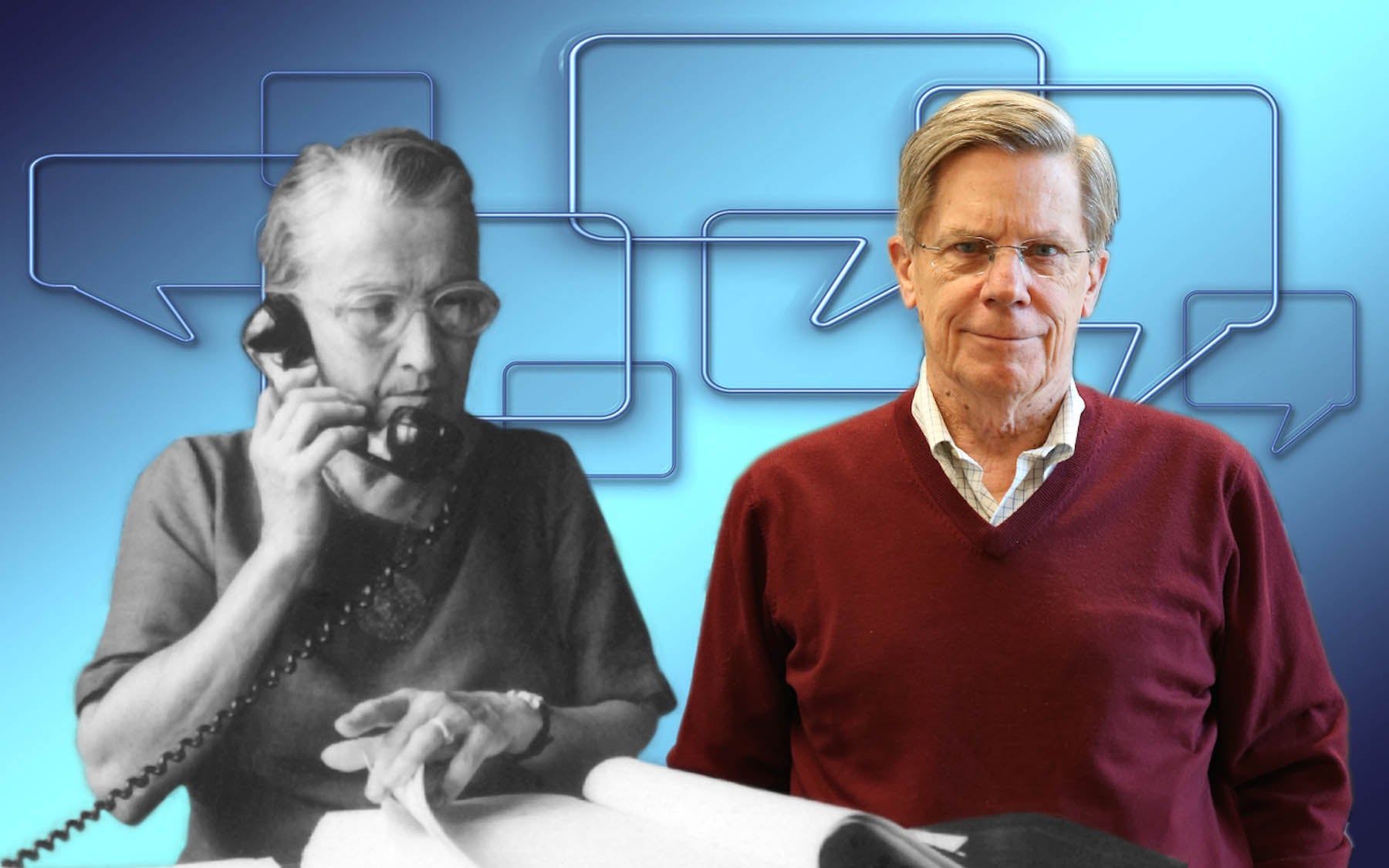
I had been aware of some new cancer immunotherapies that were in the works like the researcher that we spoke to in that full episode. Doug Fearon is working on a new cancer immuno therapy for pancreatic and colorectal cancer, but what I did not realize is that cancer immunotherapy has a much longer history than the past few years or so.
BS: Right. When we were researching this episode I was fortunate enough to stumble upon this amazing story about the fellow who is now considered the father of immunotherapy. His name was William B Coley. At the time, he didn’t know what he was doing. He didn’t know it was immunotherapy and this is in the, believe it or not, the mid 1800s. They didn’t even know what an immune system was, but he was going around infecting dying cancer patients with bacteria, which-
AA: Seems like the opposite of what you would want to do. Like, aren’t we trying to protect the compromised immune systems of cancer patients?
BS: Right. Not trying to make these people sicker, but that’s exactly what he was trying to do. Is, make these people sicker. So sick in fact, that their immune system flares up and tries to attack all the invaders in the body. It basically goes on high alert and sometimes it was a really successful approach, sometimes it totally wiped out the cancer along with the bacteria in this patient overnight. But, unfortunately the idea behind this became overshadowed by other strategies like chemotherapy and was kind of forgotten until Coley’s daughter, Hellen Coley Nauts discovered all of his noted and what not in the family barn sometime during the Great Depression. I spoke to Pete Coley, who is her nephew about what she was like and what she decided to do about this discovery.
Pete Coley: Helen is an unsung heroine who actually gathered up enough evidence to get more money going down more academic and governmental research. She learned how to write up case histories, not many people do that well. She was trained at the academy of medicine, she trudged up there practically every day from her apartment on 92nd and Madison. She’d go all the way up to 110th and 5th and educated herself. She corresponded with folks all over the world, but … Anyway, I watched her do this. Even when I was in college and after that, I would help her write her fundraising brochures and stuff like that. Finally, she teamed up with Oliver Grace of the Grace Company and they started the Cancer Research Institute in 1953. But, I remember that it all happened in her dining room.
AA: Wow. That is an amazing story. I’m so glad that she made sure that these records got the attention that they deserved.
BS: Right. Helen and the case studies she wrote up really got the ball rolling for immunotherapy, spread the word about it. Obviously, it wasn’t just the Cancer Research Institute that led it to become such a big buzzword, but she was definitely one of the big movers and shakers from that time.
AA: Back in the time of the Coleys, immunotherapy research was really based on trial and error. These observations of, “What happens if I infect this cancer patient with this bacteria? Does it work or does it not?” Trying to glean whatever insights they could off of these kind of just naked eye observations, but now scientists are able to look at cancer at the molecular level. Look into the genome, figure out the nuts and bolts behind what’s going on and why a treatment does or doesn’t work. That is what Professor Doug Fearon, who we spoke to in the full episode is really trying to do. He’s all about learning the rules of the immune system and how cancer plays into those rules. When I talked to Doug he told me something that I hadn’t really considered before, but that really made a lot of sense.
Doug Fearon: Melanoma has a lot of mutations and therefore it is more foreign than tumors that do not have a lot of mutations. It’s easier for the immune system to distinguish melanoma cancer cells from normal cells and therefore it’s easier to promote an immune attack. There’s already and ongoing low grade immune attack and you’re just promoting it. The challenge is treating cancers that have very low mutational burden and don’t have a lot of neoantigens. That’s what the field is focusing on now. It turned out that many colorectal cancer patients and pancreatic cancer patients have low numbers of mutations that do not respond to contemporary immunotherapy and that’s what we’re trying to attack.
AA: Okay. The success of immunotherapy has a lot to do with the kind of load of mutations?
Doug Fearon: The low hanging fruit has been people have already gotten that.
BS: When I heard Doug say this it made me realize that, “Oh. He is taking it a step forward than just saying, ‘Oh. This immunotherapy works and this immunotherapy doesn’t work.’” Et cetera. It’s actually, the same immunotherapy could have a different impact depending on what kind of cancer they’re using it for. Right? Am I interpreting this right?
AA: Yeah. Right. The problem with cancer or part of it at least is that cancer cells look a lot like the body’s own cells, because that’s what they started out as. They’re just the body’s own cells kind of gone rouge. But, different types of cancers can look really different at the genetic level and that means that they look different to the immune system too. When a cancer has more mutations, that tends to make it look more foreign. It’s producing more messed up gene products that the immune system can pick up on, potentially.
BS: Right. That’s what the immune system’s all about, is attacking foreign bodies. Not just cancer, not just heavily mutated cells, but really anything foreign. Like say, a tiny submarine.
AA: Yeah. Brian is not just bringing up tiny submarines out of nowhere, that’s because our resident pop culture aficionado, Sara Roncero-Menendez is here to tell us about how that tiny submarine got there.
SRM: Hey, guys.
AA: Hello, Sara.
BS: Hey. Hey.
SRM: Have you ever watched a TV show and suddenly they have this episode where the character shrink down really, really small and go inside someone else’s body?
AA: Yes. I definitely remember the Rugrats episode where they shrink down to get the watermelon seed out of Chuckie’s little belly.
SRM: Right. It’s a pretty popular formula for kids shows and for adult shows, but it actually mostly stems from this 1966 movie, “Fantastic Voyage” in which a group of scientists shrink down and get inside a tiny submarine in order to save the life of another scientist.
AA: I bet that set of some alarms within the immune system?
SRM: Oh. You betcha. In fact, one of the scientists actually dies, because white blood cells surround and kill him.
BS: Oh. The white blood cell. You mean, the great white of the immune system. Seriously though, it’s a very commonly portrayed immune system cell and I’m assuming it’s the one that you’re gonna be talking about the most?
SRM: Yep. Absolutely. In fact, it’s so infamous in the media landscape there is actually a named trope for it. It’s called, “The seeker white blood cells.” That’s when in one of these episodes the characters involved are confronted by these guardians of the body and have to deal with them in one way or another. One of these examples is from a show that you’ve probably heard something about. It’s everyone’s favorite classic science education show, “The Magic School Bus.”
BS: Yeah. That takes me back.
SRM: In fact, The Magic School Bus has not one, but three different episodes in which Ms. Frizzle and her class go inside the human body.
BS: Three? You’re kidding me. I probably lumped them all together.
SRM: Right. Well, they actually end up talking about different aspects, but the very first episode in which they do so is the one that I want to focus on today. It’s called, “Inside Ralphie.” It takes place when one of Ms. Frizzle’s students, Ralphie gets a bacterial infection and feels really sick. They decide, why not tape the action for their broadcast day by shrinking the magic school bus down really tiny and going inside or Ralphie to see what’s wrong? When they get to Ralphie’s throat they realize that it’s a bacterial infection that’s destroying the cells inside, and then “Dun-da-da.” arrive the white blood cells to fight the bacterial infection.
Speaker 7: Oh, no. Ralphie’s antibodies will mark the bus as bacteria.
Speaker 8: But, we’re not bacteria, we’re Ralphie’s friends.
Ms. Frizzle: But, his white blood cells are doing such a good job they now recognize us as enemies too.
Arnold: Enemies? But, we know what white blood cells do to enemies.
Ms. Frizzle: That’s right Arnold, they’ll try to destroy us.
Group: Destroy us?
Ms. Frizzle: Oh. The wonder of the human body.
AA: I can see why Ms. Frizzle is so psyched about the immune system coming and attacking them, because the immune system is really awesome for protecting us so well. It would be really alarming if it didn’t go after this hunk of metal and foreign humans inside of poor Ralphie’s throat.
BS: Hunk of metal and magic Andrea. It’s magic.
AA: Hunk of metal and magic. Right.
SRM: Yeah. When the white blood cell covers the bus the kids should be very, very afraid, because the white blood cell is very, very good at its job. Speaking of jobs, there is also a much less literal interpretation, but still somewhat accurate to what a white blood cell does in the movie, “Osmosis Jones.” In that movie they treat the body like it’s its own city and that make the white blood cells the police force.
Osmosis Jones: Yo. You see this badge? You see this gun? You see this gooey white sackous membranous around my personhood?
White Blood Cell: Here we go again.
Osmosis Jones: Well, you’re dealing with a white blood cell here. I should be out in the veins fighting disease, not in the mouth on tartar control.
White Blood Cell: You’re lucky you ain’t in a scab.
AA: Okay. Osmosis Jones is showing us the situation from the other side where he’s a frustrated white blood cell just trying to do his job and he feels like he’s not where the action is.
BS: Right. That’s kind of cool, because it makes you realize that the immune system is not just in your blood, it’s everywhere. Even the mouth, taking on gingivitis.
SRM: It certainly gives us a different way of visualizing just how important the white blood cells are to the maintenance of the body, in fact it is actually kind of interesting that these entertainers do understand … If in a broad sense, how the immune system works to keep us healthy.
AA: Yeah. I’m really impressed, to be honest. Especially, after our last chat episode where we saw mad scientists who feel like they’ve got everything all figured out, but don’t.
BS: Just flat don’t.
SRM: They just don’t.
AA: But, yeah. These TV shows and movies, they really used the immune system’s tenacity as part of their narrative as opposed to just ignoring the fact that if you throw a school bus, or a submarine, or a helicopter, or whatever into the body that the immune system is probably going to take note of that.
BS: Cool. That’s it.
SRM: That’s it.
BS: We’re done. If you guys have any questions, comments, please be sure to let us know. You can even leave a review on iTunes. Stay tuned for next month, we’ve got a great episode coming out and it’s gonna touch on the subject of biofuels.
AA: And how the world’s smallest flower is involved.
BS: Spoilers. Stay tuned.
AA: We’re coming to you from Cold Spring Harbor Laboratory, a private, not for profit institution at the forefront of molecular biology and genetics. If you’d like to support the research that goes on here you can find out how to do that at, “CSHL.EDU.” While you’re there, you can check out our newsstand, which showcases our videos, photos, interactive stories, and more.
BS: If that’s still not enough, you can always pay us a visit. Between our undergraduate research program, high school partnerships, graduate school, meetings and courses, and public events there really is something for everyone.
AA: I’m Andrea.
BS: I’m Brian.
SRM: I’m Sara.
AA: This is Base Pairs. More science stories soon.