Cold Spring Harbor Laboratory (CSHL) researchers led by Daniel Nolan and Assistant Professor Vivek Mittal have found that bone marrow (BM) derived endothelial progenitor cells (EPCs) play a critical role in the early stages of tumor progression and that eliminating EPCs stops cancer growth. Using sophisticated high-resolution microscopy and flow cytometry, they zeroed in on the earliest stages of cancer progression and identified the role of EPCs in generating blood vessels that allow cancers to grow. “If we selectively blocked the EPCs, tumors were unable to make blood vessels and could not sustain their own growth,” said Vivek Mittal, CSHL Assistant Professor.
The findings open an entirely new field of research on how vascular progenitor cells control tumor growth and underscore their potential for cancer therapeutics. Published on June 15, 2007 in Genes & Development, the CSHL study settles a dispute in the field of angiogenesis that has resulted from years of inconsistent findings about the existence of EPCs in cancer tumors. Until now, this field of research that focuses on new blood vessel development has been split between researchers who have suggested the existence of EPCs and those who have vehemently disputed their presence.
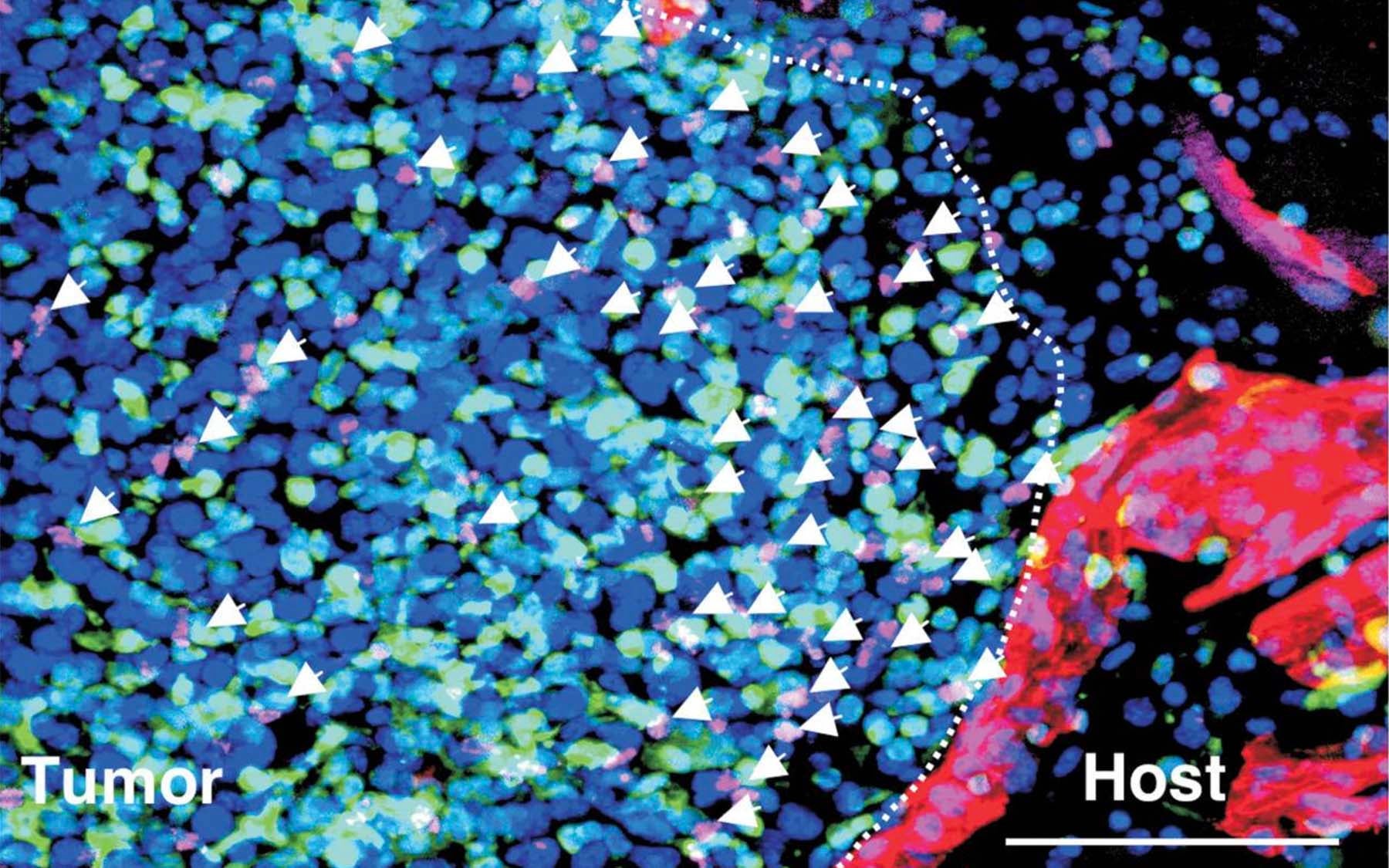
The CSHL research posits that those who did not find evidence of EPCs in tumors were probably looking for them in later stages of tumor progression when EPCs are diluted by host endothelial cells. The new results show that EPCs are only present in the earliest stages of tumor progression, before the formation of blood vessels. “We found that the role of EPCs is to direct the formation and organization of the vascular structure that ultimately feeds the tumor as it grows,” said CSHL researcher Daniel Nolan.
Using antibodies developed for angiogenic cancer treatment, CSHL researchers collaborated with Memorial Sloan-Kettering Cancer Center (MSKCC) and were able to remove EPCs without harming normal blood vessels. This has significant clinical potential, particularly in fighting cancer re-growth after incomplete surgical resection or chemotherapy. “The exciting news is that targeting such a minor population of the BM-derived tumor microenvironment has such a dramatic impact on tumor progression,” said Mittal. The study makes clear that in addition to developing therapies that directly target cancer cells, it is also equally important to develop therapies that target critical non-cancer cells like EPCs.
Written by: Communications Department | publicaffairs@cshl.edu | 516-367-8455
Citation
“Bone marrow-derived endothelial progenitor cells are a major determinant of nascent tumor neovascularization,” Daniel J. Nolan, Alessia Ciarrocchi, Albert S. Mellick, Jaspreet S. Jaggi, Kathryn Bambino, Sunita Gupta, Emily Heikamp, Michael R. McDevitt, David A. Scheinberg, Robert Benezra and Vivek Mittal.